Anal fistulas are one of the most common anorectal diseases. Treatment for anal fistulas depends on the location and complexity of the anal fistula. Surgical removal of the fistula is often required.
Read on to learn more about anal fistulas, including their causes, diagnostic process, and treatments.
An anal fistula is a small tube that begins in the anal canal on the inside and ends in the perianal skin on the outside.
Most often, this tunnel is caused by drainage from an anal abscess. An anal abscess is a collection of infected pus that forms in the rectum or anus.
Learn more about abscesses, including symptoms and treatments.
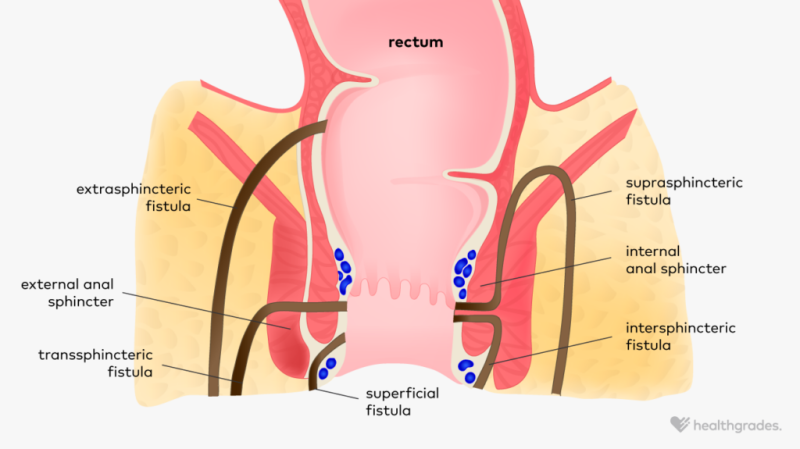
The anus has two sphincter muscles in the body to control its movements. One is internal and the other is external.doctor
trusted sources
pubmed central
National Institutes of Health’s highly respected database
Go to source
Anal fistulas differ depending on where the formed channel develops and ends.
The type of anal fistula also helps determine the treatment options your doctor recommends.
The symptoms of an anal fistula are similar to those of an anal abscess. If symptoms appear after draining an anal abscess, probably Indicates an anal fistula.
Symptoms of hemorrhoids include:
- Redness and swelling of the skin around the anus
- throbbing pain in the anal area
- Foul-smelling drainage from an opening near the anus
- blood in stool
- painful defecation
- Problems with bowel control
If you have symptoms of an anal fistula or anal abscess, contact your doctor immediately. Rapid diagnosis improves treatment outcomes and reduces the risk of complications.
Learn about other possible causes of rectal discharge.
Anal fistulas can develop for various reasons. Anal abscesses are the most common cause of anal fistulas.
in in most cases, people with anal fistulas have a history of anal abscesses. According to one report, up to 70% of people diagnosed with anal abscess also already have anal fistulas.
trusted sources
pubmed central
National Institutes of Health’s highly respected database
Go to source
.
Certain conditions that can cause inflammation in the anorectal area can also lead to the development of an anal abscess that forms a fistula. These include:
- crohn’s disease
- diverticulitis
- tuberculosis
- Trauma to the community
- Cancer and certain cancer treatments such as radiation
- sexually transmitted infections (STIs)
- Structural differences present at birth
Some anal fistulas occur naturally.
Learn more about the potential complications of Crohn’s disease.
according to
trusted sources
pubmed central
National Institutes of Health’s highly respected database
Go to source
, researchers identified trends and risk factors associated with the development of anal fistulas. These include:
- Male gender assigned at birth because males develop anal fistulas more than twice as often as females assigned at birth.
- Age ranges from 20 to 40 years, average age at diagnosis is 38 years
- hyperlipidemia, a condition in which there is a high concentration of fats or lipids in the blood
- obesity
- smoking
- Diabetes
- A life without physical activity
Talk to your doctor about your personal risk for hemorrhoids and the steps you can take to lower your risk.
To diagnose an anal fistula, your doctor will first discuss your medical history and symptoms.
The doctor will perform a physical examination of the outside and inside of the anus.This test can be uncomfortable, so your doctor may
trusted sources
pubmed central
National Institutes of Health’s highly respected database
Go to source
If it is done in the operating room, you will be under general anesthesia.
Tests that your doctor may order to diagnose and evaluate anal fistulas include:
- Digital rectal examination. This is a test in which the doctor inserts a finger to feel for changes in the structure of the anal tissue.
- Anoscopy or sigmoidoscopy. The doctor inserts a thin, flexible tube with a camera to view the lining of the anus and rectum.
- Endoanal ultrasound to help doctors find and evaluate fistulas
- Pelvic MRI, helps map the path of the fistula
- CT scan helps evaluate more complex fistulas
- Colonoscopy, if there is a fistula perhaps related to Crohn’s disease
Your doctor will discuss your diagnosis and how it determines treatment options with you.

The most common treatment for anal fistulas is traditionally surgery. However, new treatment options may also be more effective with fewer associated risks.
One of the long-standing treatments for anal fistulas is fistulotomy. This procedure involves making an incision and removing the infected area. The surgeon then sutures the area to allow it to heal.
According to , the success rate of fistulotomy is very high, up to 97%. American Society of Colorectal Surgeons (ASCRS). However, this procedure carries the risk of damaging the anal muscles that control bowel movements. This can lead to fecal incontinence.
trusted sources
pubmed central
National Institutes of Health’s highly respected database
Go to source
There is no need to cut or divide the anal muscles. These options can reduce your risk of incontinence.
- Intraanal advancement flap: This procedure involves covering the fistula opening with healthy tissue. There is still a risk of incontinence, and certain conditions can affect overall effectiveness.
- Intersphincteric fistula ligation (LIFT): This is a minimally invasive procedure that fuses and closes internal openings. In some cases, your doctor will perform the lift procedure after another procedure called seton placement.
- Seaton placement: A seton is a thin tube that your doctor inserts into your fistula. Then tie the ends on the outside of your body. This creates a loop that collects drainage while also promoting healing of the fistula.
- Fibrin glue: This procedure uses a synthetic mixture of collagen to form a plug at the inner end of the fistula. Success rates vary and further research is needed.
The ASCRS notes that drug therapy, rather than surgery, is the first-line treatment for people who develop anal fistulas due to Crohn’s disease.
An anal fistula is an abnormal tube formation that connects the inner anal canal to the outer skin. It is most commonly a complication of anal abscess.
Symptoms of an anal fistula include severe pain, redness, swelling, discharge, and bloody stools. Consult your doctor about symptoms of hemorrhoids. We can discuss prompt treatment options, including surgical excision.
