Samantha Aluko wears a color-coded hospital ID wristband long after she leaves the hospital. They serve as a fashion statement, a badge of honor, and a conversation starter to raise her awareness about ulcerative colitis.
“I have a lot,” Samantha said.
“She doesn’t want her teeth cut after she leaves the hospital,” added her mother, Nicole Arco.
Color-coded wristbands notify hospital healthcare providers of important patient details. Some are red allergy warnings (Samantha is allergic to cashews and hazelnuts). The white band has a scannable code to access medical records and patient details. In addition, hospitals may use green, blue, or other colors standardized by the hospital to match the medical condition.
Ten-year-old Samantha recalls safely passing through a checkpoint during an unexpected “mileage” journey at Phoenix Children’s. This journey gained national attention for helping her other children with her illness.
Samantha said: “I know my way around the hospital. I really know my way around the hospital, from clinics and clinics to surgeries and infusion centres.”
Her journey began when Samantha was eight years old. In August 2021, she took a crash course in her ABCs of IBD. inflammatory bowel disease. Immune system diseases cause chronic inflammation (redness and swelling) and damage to the gastrointestinal (GI) tract. It can be inherited, but the exact cause is unknown. Although there is no cure, treatment can help manage symptoms.
Crohn’s disease and ulcerative colitis are the main types of IBD. Samantha has ulcerative colitis. Crohn’s disease causes inflammation of the lower intestines (colon and rectum), but Crohn’s disease can affect any part of the gastrointestinal tract. Symptoms of IBD include abdominal pain, rectal bleeding, and bowel incontinence with an urgent need to defecate.
My third year school year got off to a bad start.
One of Samantha’s more embarrassing experiences occurred on her first day back at school, before she was diagnosed with IBD. Her classroom activities were interrupted as she made a mad dash to the bathroom.
Earlier that month, Samantha was ignoring random symptoms at home. She had mild blood and mucus in her stool, felt “gassy” and had sudden urges to go to the bathroom. But her symptoms were mild and occasional, so she wasn’t worried. After her unpleasant school days, Samantha’s symptoms quickly worsened, with more obvious rectal bleeding and gastrointestinal discomfort.
looking for answers
Samantha’s pediatrician suspected ulcerative colitis.
“This is the first time I’ve heard of it,” Nicole said. They were referred to a gastroenterologist (gastrointestinal specialist). Brad Pasternak, MD, scheduled a magnetic resonance enterography (MRE), which provides detailed pictures of the intestines. Samantha also underwent a colonoscopy. The doctor uses a long, flexible tube and a small, lighted camera to examine the colon.
Samantha said she underwent “a lot” of tests, including blood draws, stool samples, imaging tests and lab tests. The day before her colonoscopy, she cut out solid foods and took a laxative to cleanse her colon. She required general anesthesia for the 30-minute day surgery.
“I stayed calm because I didn’t want to cry,” Samantha recalled. “It was difficult, but I tried to think of positive things, like knowing that this would lead to the answer.”
Dr. Pasternak confirmed the diagnosis of ulcerative colitis. It will change the lives of a busy Phoenix-based family. Nicole and her husband Mike are the proud parents of her two daughters and fans of her family dog, Scruffy.
Natalie (Samantha’s sister, who is one year older) loves school and theater. Her credits include playing Ariel in The Little Mermaid and Olaf in Frozen. A member of her student council, Samantha loves math, reading, and science. She is a club soccer player and a Girl Scout. Their full schedule soon became even busier.
A family detour into uncharted territory
After her diagnosis, her symptoms flared up and her daily life was interrupted by medical appointments.
“It was overwhelming,” Nicole said. “You’re trying to understand this condition and you’re trying to understand how to help your child. His first year was very difficult to find the right medication.”
Samantha initially took oral steroids to relieve the inflammation. This caused her cheek to swell and required a Dexa scan to rule out complications with her bones. She then started taking oral medication, which had no effect after six weeks. Injectable medications helped her manage her symptoms for a year before failing.
“Every four to six months, I had to increase the dose or try a different drug,” Nichol said.
Samantha visits the Phoenix Pediatric Infusion Center every six weeks for IV therapy. It’s working, but Samantha is worried about it happening again.
Learn new things and have new friends lead the way
Samantha felt scared at first, but was lucky to have support.
“Everyone was great,” Samantha said. “We take each day seriously.”
She is grateful to Dr. Pasternak and others at Phoenix Children’s for making their lives a little easier.
“At first, I’m wary of new doctors,” Samantha said. “Are they friendly or tough or don’t want to talk? I got to know Dr. Pasternak very well right away. He’s always part of things. Just in hospital scrubs and a mask. It’s nice to see him at activities and events instead.”
“Dr. Pasternak will answer our questions and concerns,” Nichol added. “He has helped Mike and I with our education and is always supportive. We are lucky to have a world-class hospital in our backyard.”
New puzzles that are difficult to solve
In late 2023, Samantha began experiencing sharp pains on one side or center of her stomach. I would suddenly feel a stabbing pain while reading a book, watching TV, or taking a walk.
“Sometimes I wake up early in the morning with pain,” Samantha said.
“Her father and I swapped shifts and stayed at Samantha’s house for the night,” Nicole added. “That way, one of us could get a good night’s sleep.”
Diagnosing the new symptoms required another colonoscopy (fourth so far) and a CT scan. Samantha was waiting for an answer again.
“There are a lot of things that could happen, but you have to stay strong,” Samantha said.
The purple star continues to rise, lighting the path for others
After receiving her diagnosis, Samantha thought about other children who may feel alone, scared, and embarrassed about IBD.
“I wanted to help others,” Samantha said. “My dad is on a lot of boards, so I thought, ‘Maybe I can do that too.'”
In 2022, Samantha founded the IBD Junior Committee at Phoenix Children’s Hospital to raise awareness, support children with IBD, and fund research for a cure.
“I wanted the kids to run it,” Samantha said.
With only eight children, they raised more than $7,000 in their first year. Their membership and success continues to grow. They create logos and t-shirt designs for fundraisers and awareness. They organize video tournaments and plan toy drives for children hospitalized with IBD. Samantha encourages “welcome distractions” like her soft and cuddly Squishmallow® and activity books.
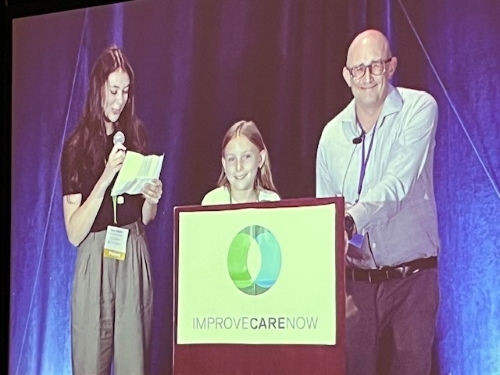
Samantha is a star among family, friends and supporters of the IBD Junior Board, but has always been a team player. When she was 10 years old, Samantha spoke at the National Pediatric Gastroenterology Conference with Dr. Pasternak on stage in a Louisville hotel ballroom.
Video of Samantha and Dr. Pasternak’s speech at the Enhanced Care Now conference in Louisville, Kentucky, October 2023: Establishment and benefits of patient-driven IBD junior committees.
“It was a proud moment,” Nicole said.
Samantha shared her story and discussed creating the board. They encouraged other children’s hospitals to form their own boards.
Samantha’s group is calling on the local mayor to light up the area purple for IBD Awareness Day in May. They have big plans and Samantha remains optimistic. She reminds others that every effort counts.
“If you want to make a difference, whatever you do is important,” Samantha said.




Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.