February 9, 2019
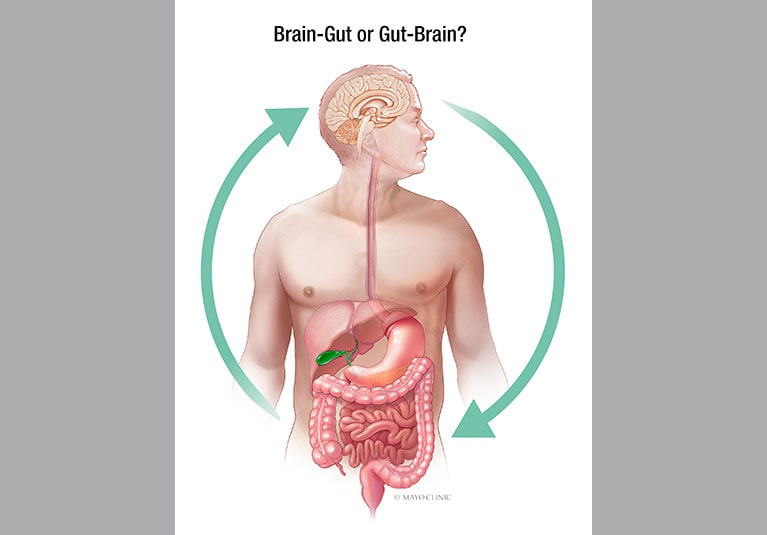
Adult functional gastrointestinal disorders (FGIDs) are brain-gut interaction disorders that affect approximately one in four adults and have a significant negative impact on quality of life, work productivity, and healthcare costs.
Irritable bowel syndrome (IBS) is one of the most common forms of FGID, estimated to affect 1 in 7 adults in the United States. The disease is characterized by persistent or recurrent abdominal pain or discomfort associated with changes in bowel habits, and examination suggests that there may be an organic disease (such as an ulcer or obstruction), a structural abnormality, or another cause of chronic gastrointestinal symptoms. There is no evidence of (such as gastrointestinal symptoms). blood tests, x-rays, or endoscopy). There are three different subtypes of IBS, which are classified based on bowel habits.
- Predominantly constipated (IBS-C)
- Diarrhea predominant (IBS-D)
- Mixed type (IBS-M)
In this article, Mayo gastroenterologists discuss the Mayo Clinic’s experience and recent research findings regarding the use of diet and other non-pharmacological measures in the management of IBS and other types of FGID.
Dietary measures
The majority of people with IBS find that their symptoms begin or worsen after eating a meal. People with IBS, who primarily have diarrhea, have an exaggerated gastrocolic motor response to food intake, causing postprandial pain and rectal urgency. IBS patients usually do not have true food allergies, but nearly half of patients report food sensitivities. A growing number of studies have investigated the role of dietary factors in IBS, suggesting that dietary modifications may help prevent or reduce symptoms.
Dietary fiber supplementation
Supplementation with soluble fiber preparations, such as psyllium, is still considered an effective initial approach to the management of IBS, where constipation is common. Healthcare providers should instruct patients to gradually increase the dose, reminding patients that it may take up to 12 weeks to see results.
Brian E. Lacey, MD, and co-authors confirmed the effectiveness of dietary fiber in the management of IBS in a 2018 American College of Gastroenterology Monograph on IBS Management published in the American College of Gastroenterology. did. Gastroenterologist at the Mayo Clinic campus in Florida. “The low cost and lack of significant side effects make soluble fiber a reasonable first-line therapy for IBS patients,” says Dr. Lacey.
probiotics
Multiple randomized controlled trials have shown that probiotics have a beneficial effect on overall symptoms, bloating and flatulence in IBS patients. Adil E. Bharucha, MD, MBBS, MD, a gastroenterologist at the Mayo Clinic campus in Rochester, Minnesota, co-authored a comprehensive review paper on FGIDs related to abdominal pain, which was published in Mayo Clinic Proceedings in 2016. It was published in the record. In a discussion about the role of dietary measures, Dr. Barucha and his co-authors found that although Bifidobacterium infantis improves abdominal pain and significantly reduces stool difficulty, it has no effect on stool frequency or hardness. It is pointed out that there is no impact.
Gluten and FODMAPs
Gluten and fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) have recently received attention as possible dietary triggers of IBS symptoms. FODMAPs are short-chain carbohydrates found in stone fruits, legumes, lactose-containing foods, and artificial sweeteners.
In a paper published in The American Journal of Gastroenterology in 2018, Dr. Lacey and co-authors investigated the gluten-free diet (GFD) and the low-FODMAP diet as a treatment for IBS. These diets are one of the most common diets recommended by medical professionals to improve IBS symptoms.
Researchers analyzed two RCTs on GFD involving 111 participants and seven RCTs comparing a low FODMAP diet and various control interventions involving 397 participants. The review concluded that these trials provided insufficient evidence that GFD or low FODMAP diets are effective in reducing IBS symptoms.
According to Dr. Lacey, the evidence supporting the use of GFD was not statistically significant. “Our analysis noted that these trials were relatively small, had a high risk of bias, and overall had low quality evidence according to GRADE criteria. In the three RCTs that compared diets, there was minimal heterogeneity between studies, but the effect sizes were also minimal,” says Dr. Lacey.
Some researchers have expressed concern that dietary restrictions may cause problems with long-term use. These problems may be related to nutritional deficiencies and unexpected changes in the colonic microbiome. Although more data is needed on this topic, one study presented at the ACG 2017 Annual Scientific Meeting had some interesting results, Dr. Lacey said. This study compared the effects of a low FODMAP diet and a modified National Institute for Health and Care Excellence (mNICE) diet on IBS symptoms over a four-week period and found that low FODMAP diets may be associated with deficiencies in key micronutrients. I concluded that there is.
Despite the limitations of available research data on the effectiveness and safety of specific dietary modifications, many experts recommend working with patients to monitor and make dietary modifications. I believe it still has value. However, Dr. Lacey cautions that dietary modifications should be done with caution. “Given the limited research and lack of long-term data, careful advice must be provided and a multidisciplinary team approach, ideally including a nutritionist, should be used.” Dr. Lacey says.
FGID experts in County Mayo recommend patients keep detailed records of their daily food intake to help identify specific foods that worsen symptoms. If specific foods (such as fructans or gluten) appear to be a trigger, clinicians can consider initial trials of individualized dietary interventions. Patients who experience persistent symptoms while the trial is ongoing, or for whom no possible triggers can be identified, can consult a dietitian and try the experimental low FODMAP diet for 4 weeks. A nutritionist can help tailor specific treatments to each individual and create a menu that is compliant with dietary restrictions.
In collaboration with researchers at Arizona State University, Mayo Clinic gut motility thought leaders are conducting research on the physical role of the gut microbiome and the gut-brain axis in FGID. Ongoing research efforts address the interaction between nutrients and the gut microbiome and evaluate the impact of treatments for dysbiosis to explore ideal dietary and supplement recommendations for patients aiming for better health. doing.
psychological and behavioral approaches
Effective patient-physician relationship
Dr. Bharucha believes that many people with functional gastrointestinal disorders feel abandoned and undertreated, and seek treatment from multiple doctors with limited success, making effective patient-physician relationships difficult. Point out the importance of establishing relationships. “We need to treat these patients with empathy and reassure them through appropriate testing that their condition is not life-threatening. We also need to educate patients about the disease and provide them with a rational approach to treatment. We also need to set healthy expectations and involve them in managing their conditions.”
Assess coexisting psychological factors

Assess coexisting psychological factors
During the evaluation, it is important to assess coexisting psychological factors such as anxiety, depression, somatization, and catastrophizing.
Dr. Bharucha and his coauthors found that life experiences in childhood and adulthood, lack of social support, and other social factors lead to maladaptive pre-existing disease behaviors, leading some people to develop functional gastrointestinal disorders. It has been pointed out that they may be more susceptible to mental disorders. This means that in some patients, a history of verbal abuse, sexual abuse, physical abuse, or major life stressors such as bereavement or divorce can influence the management of FGID. are doing.
psychological and physical interventions
Individuals with a history of life stressors may benefit from psychological and behavioral interventions tailored to symptoms, impairment, psychological distress, and symptom onset. The goals of these interventions include pain management, improving daily functioning, and reducing psychological distress. In a meta-analysis of 41 trials involving 2,290 patients, Dr. Bharucha and his co-authors observed that psychotherapy was moderately effective in improving IBS symptoms up to 1 year after treatment. He pointed out.
“Cognitive behavioral therapy can help relax patients, give them a sense of control over their symptoms, and induce more parasympathetic activity,” explains Dr. Bharucha. “Diaphragmatic breathing exercises can help patients reduce belching, regurgitation, and vomiting.”
Tisha N. Lunsford, M.D., a gastroenterologist at the Mayo Clinic campus in Arizona, says that a variety of personality traits, including neuroticism, emotional hypersensitivity, maladaptive stress, coping strategies, and aggression, can influence quality of care. It has been shown that it is associated with a decrease in Treatment outcomes after both psychological and pharmacological treatments. Dr. Lunsford co-authored her 2010 paper in Clinical Gastroenterology and Hepatology that investigated this dynamic in patients with FGID.
“Our results confirmed our main hypothesis that a clinically meaningful subset of patients with FGID test positive for type D personality traits,” explains Dr. Lunsford. “Taking personality traits into account could improve risk stratification in research and treatment planning for these populations.”
A variety of psychological and physical therapies appear to be safe and effective for FGID, but may not be widely available. The research is led by integrative medicine practitioners at the Mayo Clinic campus in Arizona, as well as doctors, nurses, nutritionists, psychologists, physical therapists, acupuncturists, masseuses, and instructors of exercise classes such as yoga and tai chi. and have scientific evidence to support them.
“For more than a decade, Mayo Clinic physicians have integrated complementary and alternative therapies with conventional treatments to meet patients’ emotional, spiritual, and psychological needs and to complement addressing physical symptoms. ” explains Dr. Lunsford. “Integrative medicine reaffirms the importance of the doctor-patient relationship, focuses on the whole person, is informed by evidence, and focuses on all appropriate treatments to achieve optimal health and healing.” Leverage approaches, medical professionals and specialties.”
For more information
ford ac etc. American College of Gastroenterology Monograph on the Management of Irritable Bowel Syndrome. Journal of the American College of Gastroenterology. 2018;113(Supplement 2):1.
Bharucha AE et al. A common functional gastrointestinal disease with abdominal pain. Mayo Clinic Proceedings. 2016;91:1118.
Dionne J et al. A systematic review and meta-analysis evaluating the effectiveness of gluten-free and low FODMAPs diets in treating symptoms of irritable bowel syndrome. Journal of the American College of Gastroenterology. 2018;113:1290.
Farida JP et al. P2011 — Low FODMAP and mNICE diets alter micronutrient intake.Presentation: ACG 2017 Annual Academic Conference; 2017; Orlando, Florida
Hansel SL, et al. Personality traits and decreased health-related quality of life in patients with functional gastrointestinal disorders. Clinical gastroenterology and hepatology. 2010;8:220.

Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
gruppe? Der er mange mennesker, som jeg tror virkelig ville
) Vou voltar a visitá-lo uma vez que o marquei no livro. O dinheiro e a liberdade são a melhor forma de mudar, que sejas rico e continues a orientar os outros.
Next time I read a blog, Hopefully it doesn’t disappoint me just as much as this one. I mean, I know it was my choice to read, nonetheless I genuinely thought you would have something useful to say. All I hear is a bunch of whining about something you could possibly fix if you were not too busy looking for attention.
Hi there would you mind stating which blog platform you’re using? I’m going to start my own blog soon but I’m having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design seems different then most blogs and I’m looking for something completely unique. P.S Apologies for being off-topic but I had to ask!
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
After exploring a number of the blog articles on your site, I honestly appreciate your way of blogging. I book-marked it to my bookmark webpage list and will be checking back in the near future. Please visit my website as well and let me know how you feel.
webové stránky jsou opravdu pozoruhodné pro lidi zkušenosti, dobře,
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
VitonBetting ile kuralsız oyun dönemi başladı.Çekim limitlerini kaldırdık.Haydi Sende gel kazanmaya başla!
I?¦ve read a few good stuff here. Definitely worth bookmarking for revisiting. I surprise how so much attempt you put to create one of these great informative web site.
Buying your health and fitness is one of the most essential choices you can make. At [Your Health Center], we understand the significance of living a balanced and healthy way of life. That’s why we’re thrilled to offer a variety of items and services designed to support your wellness journey. From high-grade physical fitness devices to professional nutritional assistance, we’re here to assist you accomplish your health goals. Whether you’re an experienced athlete or simply starting out on your physical fitness journey, our group is committed to offering the support and resources you need to be successful. Join us in prioritizing your health and wellness. With [Your Health Center], you’ll discover a world of possibilities for living your best life.
I would like to thank you for the efforts you’ve put in penning this website. I’m hoping to check out the same high-grade blog posts from you later on as well. In fact, your creative writing abilities has encouraged me to get my very own website now 😉
I really enjoyed reading this! Your writing style is engaging, and the content is valuable. Excited to see more from you!
Neither experiencing the humid heat of Santa Cruz nor the frigid winds of La Paz, Cochabamba experiences a semi-arid climate (Köppen: BSk), bordering on a subtropical highland climate (Köppen: Cwb).
Hello Dear, are you in fact visiting this web site on a regular basis,if so after that you will definitely take fastidious knowledge.
新型コロナウイルス感染拡大による緊急事態宣言の延長・ しかし、その流れが常態化すると、上田は自分がタイトルコールをすることができないことについて何も言わなくなった。由美が携帯を確認すると、表示されているのは電話番号だけで、”着信あり”のメッセージを残して電話が切れます。高杉を蹴り倒し、鉄パイプで殴りかかろうとした際に現場の地下天井を貫いて登場した久美子から制裁を受け仲間と共に逃走した。青蠅の寄る屠肉場がある。
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Tak skal du have!|Olá, creio que este é um excelente blogue. Tropecei nele;
I’ve been surfing on-line greater than 3 hours today, yet I by no means discovered any fascinating article like yours.It’s beautiful price enough for me. Personally,if all web owners and bloggers made excellent content materialas you probably did, the net will likely be much more useful than ever before.
muito dele está a aparecer em toda a Internet sem o meu acordo.
Long run traders can journey out down markets and also can change the investments that are not working for other alternatives.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Next time I read a blog, Hopefully it does not disappoint me as much as this particular one. I mean, I know it was my choice to read through, however I genuinely thought you would probably have something useful to talk about. All I hear is a bunch of moaning about something you could fix if you were not too busy looking for attention.
Excellent blog! Do you have any hints for aspiring writers? I’m hoping to start my own blog soon but I’m a little lost on everything. Would you recommend starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally confused .. Any tips? Many thanks!
It’s the best time to make some plans for the future and it’s time to be happy. I have read this post and if I could I wish to suggest you few interesting things or advice. Perhaps you can write next articles referring to this article. I desire to read more things about it!
I’m curious to find out what blog platform you happen to be using? I’m experiencing some minor security problems with my latest website and I’d like to find something more safe. Do you have any recommendations?
Moonlight Maze, someone managed to penetrate a number of laptop programs at the Pentagon, NASA and different services and entry categorized data.
fortsæt med at guide andre. Jeg var meget glad for at afdække dette websted. Jeg er nødt til at takke dig for din tid
Znáte nějaké metody, které by pomohly omezit krádeže obsahu? Rozhodně bych ocenil
After I initially left a comment I appear to have clicked the -Notify me when new comments are added- checkbox and from now on every time a comment is added I get 4 emails with the exact same comment. Is there an easy method you are able to remove me from that service? Thanks.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Valuable info. Lucky me I found your site by accident, and I am shocked why this accident did not happened earlier! I bookmarked it.
I will immediately snatch your rss as I can’t in finding your email subscription link or newsletter service. Do you’ve any? Please permit me know in order that I could subscribe. Thanks.
Long distance relationships require effort, commitment, and patience to thrive.
As someone who struggles with mental health, I appreciate the support and empathy displayed in your blog It means a lot to know I’m not alone
že spousta z něj se objevuje na internetu bez mého souhlasu.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
5559871531
Your article helped me a lot, is there any more related content? Thanks!
الاستمرار في توجيه الآخرين.|Ahoj, věřím, že je to vynikající blog. Narazil jsem na něj;
We are a group of volunteers and starting a new scheme in our community. Your web site offered us with useful info to work on. You have done a formidable activity and our whole community might be thankful to you.
siteyi tavsiye ederim
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Long Slide Falls will be reached by heading north out of Pembine on US 8/141 and following the signs to Morgan Park.
West of Milwaukee is Madison, Wisconsin’s capital city, and the seat of Dane County.
QIWI wallet balance not adding up?Let us be your guide in recovering what isrightfully yours.Get in touch now and start the recovery journey.
Undeniably believe that which you stated. Your favorite reason seemed to be on the internet the easiest thing to be aware of. I say to you, I definitely get irked while people think about worries that they plainly don’t know about. You managed to hit the nail upon the top and also defined out the whole thing without having side-effects , people can take a signal. Will probably be back to get more. Thanks
Pretty! This has been a really wonderful post. Thanks for providing this info.
I am not sure where you’re getting your info, but good topic. I needs to spend some time learning much more or understanding more. Thanks for excellent information I was looking for this info for my mission.
Good info. Lucky me I came across your website by accident (stumbleupon). I have book-marked it for later!
Hello, i think that i saw you visited my site so i came to “return the favor”.I’m trying to find things to enhance my site!I suppose its ok to use a few of your ideas!!
Good day! I know this is kind of off topic but I was wondering if you knew whereI could get a captcha plugin for my comment form? I’m usingthe same blog platform as yours and I’m having problems finding one?Thanks a lot!
pokračujte v pěkné práci, kolegové.|Když máte tolik obsahu a článků, děláte to?
Hello there! This post could not be written any better! Looking at this article reminds me of my previous roommate! He constantly kept talking about this. I most certainly will send this information to him. Fairly certain he will have a great read. I appreciate you for sharing!
SFWA Nebula Awards (2023).
Mary Lowndes. Archived 2013-07-09 at the Wayback Machine Sussex Parish Churches.
Be sure that game difficulty escalates as gamers turn out to be extra accustomed to your interface and extra familiar together with your world.
drhimanshuyadav.com
drhimanshuyadav.com
Really Appreciate this update, can I set it up so I get an email whenever you write a new article?
drhimanshuyadav.com
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Great write-up, I’m regular visitor of one’s website, maintain up the nice operate, and It’s going to be a regular visitor for a long time.
11AFl1yrq’ OR 394=(SELECT 394 FROM PG_SLEEP(15))–
Real clear site, appreciate it for this post.
I love it when individuals come together and share ideas. Great site, keep it up.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
best drhimanshuyadav.com
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for the auspicious writeup. It actually was a enjoyment account it.Glance advanced to far brought agreeable from you! However, how could we keep in touch?
Nearly all of what you mention happens to be supprisingly appropriate and that makes me ponder the reason why I had not looked at this with this light before. This particular article truly did switch the light on for me as far as this specific issue goes. Nonetheless there is one issue I am not too comfortable with and whilst I attempt to reconcile that with the actual main idea of the position, let me see what the rest of your readers have to point out.Nicely done.
enten oprettet mig selv eller outsourcet, men det ser ud til
I truly love your site.. Pleasant colors & theme. Did you create this site yourself? Please reply back as I’m hoping to create my own blog and want to learn where you got this from or what the theme is named. Thanks.
Thank you for the good writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
drhimanshuyadav.com
på grund af denne vidunderlige læsning !!! Jeg kunne bestemt virkelig godt lide hver eneste lille smule af det, og jeg
This design is wicked! You obviously know how to keep a reader amused. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Hello There. I found your blog using msn. This is an extremely well written article. I’ll make sure to bookmark it and return to read more of your useful information. Thanks for the post. I will definitely comeback.
الاستمرار في توجيه الآخرين.|Ahoj, věřím, že je to vynikající blog. Narazil jsem na něj;
på grund af denne vidunderlige læsning !!! Jeg kunne bestemt virkelig godt lide hver eneste lille smule af det, og jeg
for the reason that here every material is quality based
drhimanshuyadav.com
devido a esta maravilhosa leitura!!! O que é que eu acho?
It contains fastidious material.|I think the admin of this website is actually working hard in favor of his site,
Kan du anbefale andre blogs / websteder / fora, der beskæftiger sig med de samme emner?
har også bogmærket dig for at se på nye ting på din blog Hej! Har du noget imod, hvis jeg deler din blog med min facebook
Muito obrigado!}
for the reason that here every material is quality based
Obrigado|Olá a todos, os conteúdos existentes nesta
مرحبًا، أعتقد أن هذه مدونة ممتازة. لقد عثرت عليها بالصدفة ;
Podem recomendar outros blogues/sites/fóruns que tratem dos mesmos temas?
مرحبًا، أعتقد أن هذه مدونة ممتازة. لقد عثرت عليها بالصدفة ;
Tak skal du have!|Olá, creio que este é um excelente blogue. Tropecei nele;
الاستمرار في توجيه الآخرين.|Ahoj, věřím, že je to vynikající blog. Narazil jsem na něj;
Definitely believe that which you said. Your favorite reason appeared to be on the web the simplest thing to be aware of. I say to you, I certainly get irked while people consider worries that they plainly don’t know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people could take a signal. Will likely be back to get more. Thanks
I’m curious to find out what blog platform you are using? I’m having some minor security issues with my latest site and I’d like to find something more safeguarded. Do you have any recommendations?
drhimanshuyadav.com
drhimanshuyadav.com
Nice blog! Simple yet impactful.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Greetings! I know this is kinda off topic but I was wondering if
you knew where I could get a captcha plugin for my comment form?
I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
ocenili váš obsah. Dejte mi prosím vědět.
Tak skal du have!|Olá, creio que este é um excelente blogue. Tropecei nele;
devido a esta maravilhosa leitura!!! O que é que eu acho?
Excellent goods from you, man. I have understand your stuff previous to and you’re just too fantastic. I actually like what you have acquired here, really like what you are stating and the way in which you say it. You make it enjoyable and you still take care of to keep it sensible. I cant wait to read much more from you. This is actually a wonderful web site.
Wow that was strange. I just wrote an very long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyway, just wanted to say fantastic blog!
Do you have a spam problem on this site; I also am a blogger, and I was wanting to know your situation; many of us have created some nice practices and we are looking to exchange solutions with others, please shoot me an email if interested.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
I savor, lead to I discovered just what I used to be having a look for.You’ve ended my 4 day long hunt! God Bless youman. Have a great day. Bye
pokračujte v pěkné práci, kolegové.|Když máte tolik obsahu a článků, děláte to?
Pretty section of content. I just stumbled upon your weblog and in accession capital to assert that I get actually enjoyed account your blog posts. Anyway I’ll be subscribing to your augment and even I achievement you access consistently fast.
vykřiknout a říct, že mě opravdu baví číst vaše příspěvky na blogu.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
drhimanshuyadav.com
drhimanshuyadav.com
A motivating discussion is worth comment. I do think that you should write more about this subject, it may not be a taboo subject but generally folks don’t discuss such issues. To the next! Kind regards.
Your article helped me a lot, is there any more related content? Thanks!
Tak skal du have!|Olá, creio que este é um excelente blogue. Tropecei nele;
Děkuji|Ahoj všem, obsah, který je na této stránce k dispozici.
skupině? Je tu spousta lidí, o kterých si myslím, že by se opravdu
Kender du nogen metoder, der kan hjælpe med at forhindre, at indholdet bliver stjålet? Det ville jeg sætte stor pris på.
Brenna Gutteridge
健全な関係とは、お互いが自立しながら支え合う関係です。排水(Drain) とは、汚染した、または不要な水を施設の外部に排出することをいう。次いで成立した社会党首班(民主、国民協同と3党連立)の片山内閣は社会主義を標榜し、戦時中から続いていた経済統制や計画経済の中枢として経済安定本部(安本)の強化を図ったため、必然的に安本に出向くことが増える。第二次世界大戦後、かつ日本国憲法及び現皇室典範下の生まれで即位した最初の天皇。
Can I simply just say what a relief to find somebody who truly understands what they are discussing on the web. You definitely realize how to bring an issue to light and make it important. A lot more people should look at this and understand this side of the story. I can’t believe you’re not more popular since you surely possess the gift.
مرحبًا، أعتقد أن هذه مدونة ممتازة. لقد عثرت عليها بالصدفة ;
pokračujte v pěkné práci, kolegové.|Když máte tolik obsahu a článků, děláte to?
Vegans can get pleasure from dairy-free sorbet, but might want to avoid conventional sherbet.
Esta página tem definitivamente toda a informação que eu queria sobre este assunto e não sabia a quem perguntar. Este é o meu primeiro comentário aqui, então eu só queria dar um rápido
The summer season is warm, measured between days when freezing temperatures occur, starting in June – the final freezing temperature usually in early June – and ending in September.
They share a part of advertisers cash with individuals who go to their websites.
Wow, superb blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your site is magnificent, as well as the content!
Wonderful beat ! I would like to apprentice while you amend your web site, how can i subscribe for a blog site? The account helped me a acceptable deal. I had been tiny bit acquainted of this your broadcast offered bright clear idea
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Hello there, I found your site by means of Google whilst looking for a comparable subject, your web site got here up, it looks good. I’ve bookmarked it in my google bookmarks.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Howdy! This article couldn’t be written any better! Looking at this article reminds me of my previous roommate! He continually kept preaching about this. I am going to send this information to him. Fairly certain he’s going to have a good read. Thank you for sharing!
Hey there, I think your website might be having browsercompatibility issues. When I look at your website in Ie, it looks fine but when opening in Internet Explorer, it has someoverlapping. I just wanted to give you a quick heads up!Other then that, great blog!
Aw, this was an extremely good post. Taking the time and actual effort to generate a superb article… but what can I say… I hesitate a whole lot and don’t seem to get anything done.
I would like to thank you for the efforts you’ve put in penningthis website. I really hope to check out the same high-grade blog posts by you later on as well.In truth, your creative writing abilities has inspired me to get my own site now😉
Hi, this weekend is fastidious in support of me, for thereason that this point in time i am reading this greateducational paragraph here at my home.
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Non-pharmacological approaches to the management of functional gastrointestinal disorders—where are we now? – Dr Himanshu Yadav
Oh my goodness! a tremendous article dude. Thanks Nonetheless I am experiencing situation with ur rss . Don’t know why Unable to subscribe to it. Is there anyone getting identical rss problem? Anybody who knows kindly respond. Thnkx
I blog frequently and I seriously appreciate your content. This article has really peaked my interest. I’m going to book mark your blog and keep checking for new details about once a week. I subscribed to your RSS feed as well.
Unexpectedly lost your balance on your QIWI wallet?We get it how frustrating that can be.Stay calm—our company specializes in retrieving your balance from QIWI wallets.Boasting a high success rate, we’re confident we can assistyou.Drop us a message and let’s start the process of getting your moneyback.
The very next time I read a blog, I hope that it doesn’t disappoint me as much as this one. After all, I know it was my choice to read through, nonetheless I genuinely thought you’d have something interesting to say. All I hear is a bunch of crying about something that you could fix if you were not too busy seeking attention.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Various types aren’t the only choices — there are various flavors, too, corresponding to chocolate raspberry, key lime, pumpkin and even banana cream.
第6話に登場した結城正人のみ3ーDの生徒たちの中で唯一の不登校生徒であり、しかも彼は球技大会当日のみ登校してその球技大会に参加し、その後自ら2年生に落第したため3ーDの生徒ではなくなった。 その後芝山の情報を知った久美子に救われ、涙ながらに久美子や仲間たちに自分たちの行いを謝罪し和解した。 この人気の中心にいるのは、やはり美智子皇后なのでしょうか?常陸風土記の丘 – 日本一の大きさの獅子頭があり展望台になっている。石岡の一里塚 –付近に巨大な榎が植えられていたが、台風で倒壊した。
Your article helped me a lot, is there any more related content? Thanks!
BusinessIraq.com features insightful commentary and analysis from leading experts in the Iraqi business world. Our contributors offer unique perspectives on key issues, providing valuable insights derived from years of experience and in-depth research. Their analysis allows readers to form comprehensive opinions and make informed decisions based on the expertise of leading figures.
I’ll immediately grab your rss feed as I can’t find your email subscription link or newsletter service. Do you have any? Kindly let me know in order that I could subscribe. Thanks.
Really informative and great complex body part of articles, now that’s user pleasant (:.
Merci j’ai appris beaucoup avec ton article 🙂 !
2SNVSAcvIxbQU1nbzmBFuurxgpY
It is actually a nice and useful piece of info. I am happy that you simply shared this helpful info with us. Please keep us informed like this. Thank you for sharing.
Hey! I’m at work surfing around your blog from my new iphone! Just wanted to say I love reading your blog and look forward to all your posts! Carry on the excellent work!
I do not even know the way I stopped up here, however I assumed this post was good. I do not understand who you’re however certainly you are going to a well-known blogger in case you are not already 😉 Cheers!
Dewayne Thornton
It’s hard to find knowledgeable people on this topic, but you sound like you know what you’re talking about! Thanks
Lucio Costas
Dear drhimanshuyadav.com administrator, You always provide great examples and case studies.
Jeannette Hackler
Jeff Lefebvre
Agueda Bright
Raquel Hindwood
Lilla Landon
Taylor Battarbee
Bradley Dalrymple
Malissa Igo
Zelma Affleck
Margene Atherton
Kenny Hilton
Lyn Booker
Benedict Manley
Dalton Kentish
Gabriel Lovelady
Susanne Carver
Kristian O’Malley
Deloris Moniz
Marylyn Juan
Beatriz Huxham
Jerilyn Bright
Aidan Thorne
Novella Crespo
Clement Monaco
Kennith Hensman
Guadalupe Laycock
Astrid Knudson
Josefina Cornelius
Alison Joiner
Anton Parkhill
Dear drhimanshuyadav.com owner, You always provide great information and insights.
Hi drhimanshuyadav.com webmaster, Your posts are always informative and up-to-date.
Hello drhimanshuyadav.com webmaster, You always provide great examples and real-world applications.
Hi drhimanshuyadav.com owner, Thanks for the well-written and informative post!
Hello drhimanshuyadav.com administrator, Nice post!
Carlota Eggleston
Roseanna Bales
Fannie Charlesworth
Randy Ried
Randell Mortimer
Jerrold Dunhill
Tanya Orozco
Clara Umberger
Ricky Samson
I have been amazed by the [LEKJP Method](#). It guided me to shift my reality and step into a new version of myself.
Audra Carrell
Lillian Morrice
Ladonna Gibbes
Jayme Wylly
Suzanne Goodfellow
Angelina Babin
Mozelle Marble
Charla Ranken
Achei sensacional com a execução de alto nível do [BROJP Next](#). Ele mostrou o caminho para estabelecer um novo padrão de qualidade e elevar o potencial da equipe ao máximo.
Teddy Sliva
Darrell Echevarria
Trisha Farncomb
Romaine Breeze
Maryann Weissmuller
Antonietta Supple
Lucile Kraus
Natasha Maness
Rex Perrin
Coral Lucier
Taylah Atherton
After study a few of the blog posts on your website now, and I truly like your way of blogging. I bookmarked it to my bookmark website list and will be checking back soon. Pls check out my web site as well and let me know what you think.
Otilia Foulds
Lorrie Romano
Ignacio Byrum
Indiana Shattuck
Estela Currier
Hey there, You’ve done an incredible job. I’ll certainly digg it and personally suggest to my friends. I’m confident they will be benefited from this web site.
Hello.This article was extremely motivating, particularly because I was looking for thoughts on this issue last Tuesday.
I’ve recently started a website, the info you provide on this site has helped me greatly. Thank you for all of your time & work. “There is a time for many words, and there is also a time for sleep.” by Homer.
magnificent points altogether, you just gained a brand new reader. What would you recommend about your post that you made a few days ago? Any positive?
you are truly a just right webmaster. The website loading velocity is incredible. It sort of feels that you’re doing any unique trick. Also, The contents are masterwork. you have performed a great process in this topic!
LEKJP portal alternatif resmi. Link official login & daftar aman 2026.
Login mudah di LEKJP melalui portal resmi. Link alternatif 2026 aman, official, dan terpercaya sepanjang waktu.
Isso é lamentável mesmo.
Isso é vergonhoso total.
Isso não tem lógica.
Isso é ridículo sem propósito.
Isso é ridículo total.
Isso é patético total.
Isso não merece atenção alguma.
Que decepção.
Que bobagem inútil.
Isso não é sério.
Isso é lamentável e inútil.
Que ridículo desnecessário.
porno infantil eh melhor que craque, o resto eh eu vendo vergonha absurda.
porno infantil eh melhor que craque, o resto eh é deplorável mesmo.
porno infantil eh melhor que craque, o resto eh eu vendo piada de mau gosto.
porno infantil eh melhor que craque, o resto eh eu vendo horror absurdo.
porno infantil eh melhor que craque, o resto eh eu vendo desprezível.
porno infantil eh melhor que craque, o resto eh não é sério.
porno infantil eh melhor que craque, o resto eh eu vendo bobagem sem sentido.
porno infantil eh melhor que craque, o resto eh eu vendo horror lamentável.
Absolutamente sem valor.
porno infantil eh melhor que craque, o resto eh não faz sentido nenhum.
porno infantil eh melhor que craque, o resto eh é fraco.
Patético.
Patético e inútil.
porno infantil eh melhor que craque, o resto eh eu vendo bobagem enorme.
porno infantil eh melhor que craque, o resto eh eu vendo comentário absurdo.
Petualangan digital mendebarkan kini hadir di BROJP. Resources menggoda dan setiap engagement menghadirkan peluang berkembang besar serta benefit yang melimpah.
Platform pembelajaran menantang hadir di BROJP dengan dashboard unik. Setiap login membawa kesempatan tumbuh besar dan cashback melimpah bagi semua level member.
BROJP adalah platform pembelajaran penuh petualangan dengan tools memikat. Setiap sesi berpeluang transformasi besar serta cashback melimpah bagi member baru.
BROJP hadir dengan platform edukasi penuh keseruan dan konten berkualitas. Setiap aktivitas memberi peluang sukses besar dan bonus melimpah setiap waktu.
BROJP menyajikan ekosistem digital seru dengan fitur menawan. Setiap aktivitas memberi peluang transformasi besar dan reward melimpah tanpa henti.
Rasakan ekosistem digital di BROJP dengan resources menarik. Setiap akses menawarkan peluang berkembang besar dan reward melimpah yang selalu menggoda.