A minimally invasive surgical approach called laparoscopic rectal mobilization and genitourinary separation appears to be a safe alternative to open surgery for eligible patients with cloacal malformations.That’s the latest conclusion study by the team of Colorectal and Pelvic Malformation Center At Boston Children’s Hospital.
Minimally invasive approach to genitourinary separation
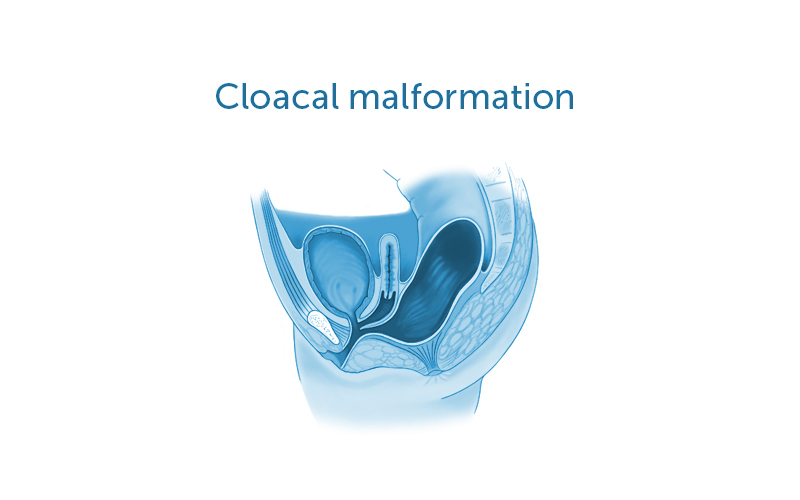
Cloacal malformation is a rare type of anorectal malformation that occurs when the structures of a girl’s rectum, vagina, and urinary system form one common passageway. The choice of surgical repair strategy largely depends on the baby’s total passageway and urethral length. Cloaca of medium to long common passages are difficult and often require laparotomy for dissection of the pelvic structures. This large surgical incision allows the surgeon to see all of the patient’s relevant anatomy, including the urinary tract, reproductive tract, and parts of the intestines. You can also separate these structures from each other to create separate openings.
Important points
- Cloacal malformations are a rare type of anorectal malformation that require surgical repair.
- Surgeons at the Boston Pediatric Colorectal Malformation Center have developed a laparoscopic approach to rectal mobilization and genitourinary separation.
- This minimally invasive approach may speed recovery, shorten hospital stay, and reduce the amount of pain medication.
- A recent study by the research team found this approach to be safe for patients with an average common channel length of 3.5 cm.
Although laparoscopy has been used for rectal dissection, it has not previously been used for the management of genitourinary structures. The center director is Belinda Dickie, MDAssociate Director, Erin McNamara, MD, MPHand colleagues recently adopted a laparoscopic approach for rectal mobilization and urogenital separation.
This minimally invasive approach allows the surgeon to obtain a close-up view of the child’s anatomy. Because the incisions required are smaller, recovery may be faster, hospital stays may be shorter, and pain medication may be required less.
Benefiting patients with a safe approach
To assess the safety of this approach, the team studied nine patients with cloacal deformities who underwent laparoscopic rectal mobilization and genitourinary separation at Boston Children’s Hospital and elsewhere between 2016 and 2019. records of children were reviewed. This included details such as patient demographics, relevant anatomical lengths, and urinary tract lengths. Surgery, blood transfusion requirements, and perioperative complications.
The research team found that the common channel length in these patients was 3.5 centimeters. There were no intraoperative complications and the need for blood transfusions was minimal. The hospitalization period was approximately 6 days. The results of this survey were published in the November 17, 2020 issue. Journal of Laparoendoscopy and Advanced Surgical Techniques.
“This minimally invasive approach provides the benefits of laparoscopic surgery by allowing us to visualize all abdominal and pelvic structures and safely separate them,” says McNamara. “We will continue to follow these patients to see if there is any improvement in other outcomes such as incontinence.”
“Our surgeons are skilled in both open and laparoscopic reconstruction of cloacal anomalies,” Dickey added. “We adapted laparoscopy because we believe it can provide the same or better results for certain patients. There are few centers in the world with such extensive experience.”
For more information, Colorectal and Pelvic Malformation Center.
