February 9, 2019
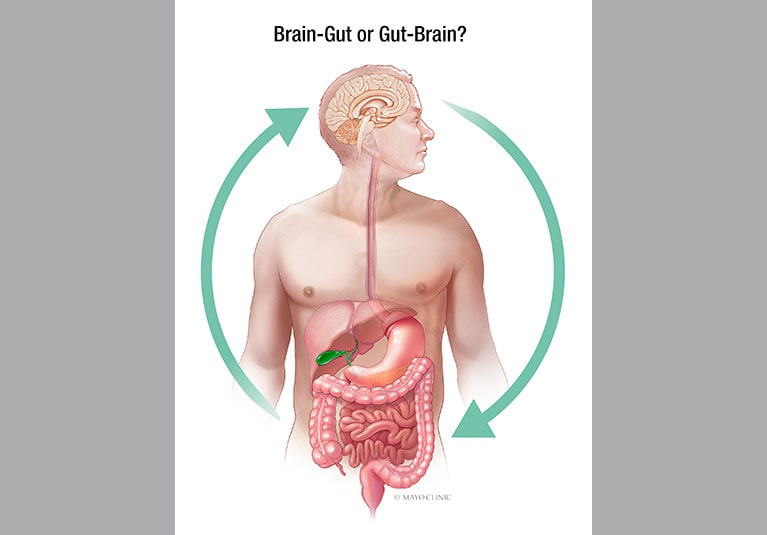
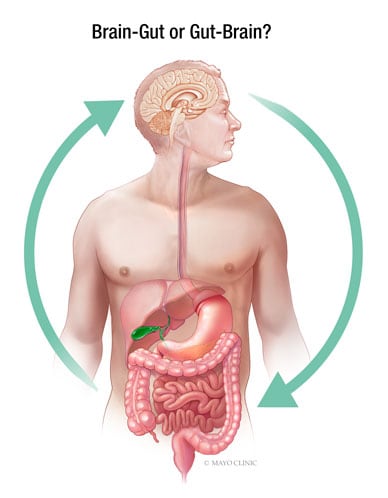
Adult functional gastrointestinal disorders (FGIDs) are brain-gut interaction disorders that affect approximately one in four adults and have a significant negative impact on quality of life, work productivity, and healthcare costs.
Irritable bowel syndrome (IBS) is one of the most common forms of FGID, estimated to affect 1 in 7 adults in the United States. The disease is characterized by persistent or recurrent abdominal pain or discomfort associated with changes in bowel habits, and examination suggests that there may be an organic disease (such as an ulcer or obstruction), a structural abnormality, or another cause of chronic gastrointestinal symptoms. There is no evidence of (such as gastrointestinal symptoms). blood tests, x-rays, or endoscopy). There are three different subtypes of IBS, which are classified based on bowel habits.
- Predominantly constipated (IBS-C)
- Diarrhea predominant (IBS-D)
- Mixed type (IBS-M)
In this article, Mayo gastroenterologists discuss the Mayo Clinic’s experience and recent research findings regarding the use of diet and other non-pharmacological measures in the management of IBS and other types of FGID.
Dietary measures
The majority of people with IBS find that their symptoms begin or worsen after eating a meal. People with IBS, who primarily have diarrhea, have an exaggerated gastrocolic motor response to food intake, causing postprandial pain and rectal urgency. IBS patients usually do not have true food allergies, but nearly half of patients report food sensitivities. A growing number of studies have investigated the role of dietary factors in IBS, suggesting that dietary modifications may help prevent or reduce symptoms.
Dietary fiber supplementation
Supplementation with soluble fiber preparations, such as psyllium, is still considered an effective initial approach to the management of IBS, where constipation is common. Healthcare providers should instruct patients to gradually increase the dose, reminding patients that it may take up to 12 weeks to see results.
Brian E. Lacey, MD, and co-authors confirmed the effectiveness of dietary fiber in the management of IBS in a 2018 American College of Gastroenterology Monograph on IBS Management published in the American College of Gastroenterology. did. Gastroenterologist at the Mayo Clinic campus in Florida. “The low cost and lack of significant side effects make soluble fiber a reasonable first-line therapy for IBS patients,” says Dr. Lacey.
probiotics
Multiple randomized controlled trials have shown that probiotics have a beneficial effect on overall symptoms, bloating and flatulence in IBS patients. Adil E. Bharucha, MD, MBBS, MD, a gastroenterologist at the Mayo Clinic campus in Rochester, Minnesota, co-authored a comprehensive review paper on FGIDs related to abdominal pain, which was published in Mayo Clinic Proceedings in 2016. It was published in the record. In a discussion about the role of dietary measures, Dr. Barucha and his co-authors found that although Bifidobacterium infantis improves abdominal pain and significantly reduces stool difficulty, it has no effect on stool frequency or hardness. It is pointed out that there is no impact.
Gluten and FODMAPs
Gluten and fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) have recently received attention as possible dietary triggers of IBS symptoms. FODMAPs are short-chain carbohydrates found in stone fruits, legumes, lactose-containing foods, and artificial sweeteners.
In a paper published in The American Journal of Gastroenterology in 2018, Dr. Lacey and co-authors investigated the gluten-free diet (GFD) and the low-FODMAP diet as a treatment for IBS. These diets are one of the most common diets recommended by medical professionals to improve IBS symptoms.
Researchers analyzed two RCTs on GFD involving 111 participants and seven RCTs comparing a low FODMAP diet and various control interventions involving 397 participants. The review concluded that these trials provided insufficient evidence that GFD or low FODMAP diets are effective in reducing IBS symptoms.
According to Dr. Lacey, the evidence supporting the use of GFD was not statistically significant. “Our analysis noted that these trials were relatively small, had a high risk of bias, and overall had low quality evidence according to GRADE criteria. In the three RCTs that compared diets, there was minimal heterogeneity between studies, but the effect sizes were also minimal,” says Dr. Lacey.
Some researchers have expressed concern that dietary restrictions may cause problems with long-term use. These problems may be related to nutritional deficiencies and unexpected changes in the colonic microbiome. Although more data is needed on this topic, one study presented at the ACG 2017 Annual Scientific Meeting had some interesting results, Dr. Lacey said. This study compared the effects of a low FODMAP diet and a modified National Institute for Health and Care Excellence (mNICE) diet on IBS symptoms over a four-week period and found that low FODMAP diets may be associated with deficiencies in key micronutrients. I concluded that there is.
Despite the limitations of available research data on the effectiveness and safety of specific dietary modifications, many experts recommend working with patients to monitor and make dietary modifications. I believe it still has value. However, Dr. Lacey cautions that dietary modifications should be done with caution. “Given the limited research and lack of long-term data, careful advice must be provided and a multidisciplinary team approach, ideally including a nutritionist, should be used.” Dr. Lacey says.
FGID experts in County Mayo recommend patients keep detailed records of their daily food intake to help identify specific foods that worsen symptoms. If specific foods (such as fructans or gluten) appear to be a trigger, clinicians can consider initial trials of individualized dietary interventions. Patients who experience persistent symptoms while the trial is ongoing, or for whom no possible triggers can be identified, can consult a dietitian and try the experimental low FODMAP diet for 4 weeks. A nutritionist can help tailor specific treatments to each individual and create a menu that is compliant with dietary restrictions.
In collaboration with researchers at Arizona State University, Mayo Clinic gut motility thought leaders are conducting research on the physical role of the gut microbiome and the gut-brain axis in FGID. Ongoing research efforts address the interaction between nutrients and the gut microbiome and evaluate the impact of treatments for dysbiosis to explore ideal dietary and supplement recommendations for patients aiming for better health. doing.
psychological and behavioral approaches
Effective patient-physician relationship
Dr. Bharucha believes that many people with functional gastrointestinal disorders feel abandoned and undertreated, and seek treatment from multiple doctors with limited success, making effective patient-physician relationships difficult. Point out the importance of establishing relationships. “We need to treat these patients with empathy and reassure them through appropriate testing that their condition is not life-threatening. We also need to educate patients about the disease and provide them with a rational approach to treatment. We also need to set healthy expectations and involve them in managing their conditions.”
Assess coexisting psychological factors
Assess coexisting psychological factors
During the evaluation, it is important to assess coexisting psychological factors such as anxiety, depression, somatization, and catastrophizing.
Dr. Bharucha and his coauthors found that life experiences in childhood and adulthood, lack of social support, and other social factors lead to maladaptive pre-existing disease behaviors, leading some people to develop functional gastrointestinal disorders. It has been pointed out that they may be more susceptible to mental disorders. This means that in some patients, a history of verbal abuse, sexual abuse, physical abuse, or major life stressors such as bereavement or divorce can influence the management of FGID. are doing.
psychological and physical interventions
Individuals with a history of life stressors may benefit from psychological and behavioral interventions tailored to symptoms, impairment, psychological distress, and symptom onset. The goals of these interventions include pain management, improving daily functioning, and reducing psychological distress. In a meta-analysis of 41 trials involving 2,290 patients, Dr. Bharucha and his co-authors observed that psychotherapy was moderately effective in improving IBS symptoms up to 1 year after treatment. He pointed out.
“Cognitive behavioral therapy can help relax patients, give them a sense of control over their symptoms, and induce more parasympathetic activity,” explains Dr. Bharucha. “Diaphragmatic breathing exercises can help patients reduce belching, regurgitation, and vomiting.”
Tisha N. Lunsford, M.D., a gastroenterologist at the Mayo Clinic campus in Arizona, says that a variety of personality traits, including neuroticism, emotional hypersensitivity, maladaptive stress, coping strategies, and aggression, can influence quality of care. It has been shown that it is associated with a decrease in Treatment outcomes after both psychological and pharmacological treatments. Dr. Lunsford co-authored her 2010 paper in Clinical Gastroenterology and Hepatology that investigated this dynamic in patients with FGID.
“Our results confirmed our primary hypothesis that a clinically meaningful subset of FGID patients test positive for Type D personality traits,” explains Dr. Lunsford. “Taking personality traits into account could improve risk stratification in research and treatment planning for these populations.”
A variety of psychological and physical therapies appear to be safe and effective for FGID, but may not be widely available. The research is led by integrative medicine practitioners at the Mayo Clinic campus in Arizona, as well as doctors, nurses, nutritionists, psychologists, physical therapists, acupuncturists, masseuses, and instructors of exercise classes such as yoga and tai chi. and have scientific evidence to support them.
“For more than a decade, Mayo Clinic physicians have integrated complementary and alternative therapies with conventional treatments to meet patients’ emotional, spiritual and psychological needs and to supplement the management of physical symptoms.” explains Dr. Lunsford. “Integrative medicine reaffirms the importance of the doctor-patient relationship, focuses on the whole person, is informed by evidence, and focuses on all appropriate treatments to achieve optimal health and healing.” Leverage approaches, medical professionals and specialties.”
For more information
ford ac etc. American College of Gastroenterology Monograph on the Management of Irritable Bowel Syndrome. Journal of the American College of Gastroenterology. 2018;113(Supplement 2):1.
Bharucha AE et al. A common functional gastrointestinal disease with abdominal pain. Mayo Clinic Proceedings. 2016;91:1118.
Dionne J et al. A systematic review and meta-analysis evaluating the effectiveness of gluten-free and low FODMAPs diets in treating symptoms of irritable bowel syndrome. Journal of the American College of Gastroenterology. 2018;113:1290.
Farida JP et al. P2011 — Micronutrient intake is altered by low FODMAP and mNICE diets.Presentation: ACG 2017 Annual Academic Conference; 2017; Orlando, Florida
Hansel SL, et al. Personality traits and decreased health-related quality of life in patients with functional gastrointestinal disorders. Clinical gastroenterology and hepatology. 2010;8:220.

Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.