
Anorectal health is an often-overlooked aspect of overall well-being. In India, conditions such as piles (bawaseer), fissures, bhagandar (anal fistula), abscesses, prolapse, and rectal bleeding can significantly impact quality of life. This comprehensive guide provides a detailed overview of these conditions, including their symptoms, causes, and effective treatment options.
Anatomy of the Anus and Rectum
The anus and rectum are essential parts of the digestive system. The rectum is the final 6-8 inches of the large intestine, and the anus is the opening through which stool is expelled.
Common Anorectal Conditions
1. Piles (Bawaseer)
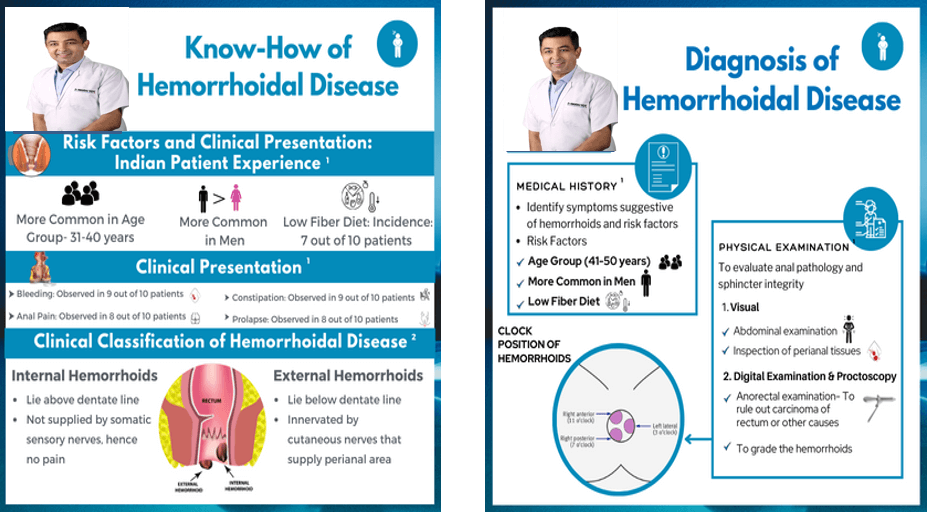
Piles, also known as hemorrhoids, are swollen veins in the rectal area. They can be classified into:
Internal Piles: Located inside the rectum.
External Piles: Located outside the anus.
Symptoms:
Itching
Pain
Bleeding during bowel movements
Classification of Piles :
Piles may be internal or external. Internal piles are further classified into grades:
Grade I – No protrusion from anus.
Grade II – Protrusion through the anus during straining and defecation, but return spontaneously.
Grade III – Protrude through the anus with defecation or straining, but manually reduced.
Grade IV – Protrude and cannot be manually reduced.
Treatment:
Lifestyle changes (increased fiber intake, regular exercise)
Over-the-counter medications (ointments, suppositories)
Surgical procedures (hemorrhoidectomy, stapler hemorrhoidopexy, rubber band ligation)
2. Anorectal Fissures
Anorectal fissures are small tears in the lining of the anus. They can be caused by passing hard stools, chronic diarrhea, or childbirth.
Symptoms:
Sharp pain during and after bowel movements
Bleeding
Treatment:
Increased fiber intake
Stool softeners
Topical medications (nitroglycerin ointment, calcium channel blockers)
Surgical procedures (lateral internal sphincterotomy)
3. Bhagandar (Anal Fistula)
An anal fistula is an abnormal tunnel that forms between the anal canal and the skin near the anus.
Opens in a new window
my.clevelandclinic.org
anal fistula
Symptoms:
Persistent discharge of pus
Pain
Swelling
Treatment:
Surgical procedures (fistulotomy, seton placement, advancement flap surgery, LIFT procedure)
4. Anorectal Abscess
An anorectal abscess is a localized infection that forms in the rectal area.
Symptoms:
Severe pain
Swelling
Fever
Treatment:
Surgical drainage of the abscess
Antibiotics
5. Rectal Prolapse
Rectal prolapse occurs when part of the rectum protrudes through the anus.
Symptoms:
Visible protrusion of the rectum
Discomfort
Incontinence
Treatment:
Surgical procedures (rectopexy)
Non-surgical treatments (pelvic floor exercises, support devices)
6. Blood Coming Out of the Anus
Blood coming out of the anus can be a symptom of various anorectal conditions. It is essential to consult a healthcare professional for proper diagnosis and treatment

Piles management can be both Medical or Surgical (LASER being the most popular)


‘LASER’ surgery offers several advantages over traditional open surgery techniques in certain cases. Here are some of the general benefits of laser surgery:
1. Precision: Laser surgery allows for precise and controlled incisions, which can be particularly advantageous when operating on delicate or sensitive tissues. The laser can selectively target the affected area while minimizing damage to surrounding healthy tissues.
2. Minimized bleeding: The laser cauterizes blood vessels as it cuts, which helps to minimize bleeding during the procedure. This reduces the need for extensive suturing and can lead to a cleaner surgical field.
3. Reduced risk of infection: The high heat generated by lasers can sterilize the surgical site, reducing the risk of infection compared to traditional open surgery.
4. Quicker recovery: Laser surgery is generally associated with smaller incisions and less tissue trauma compared to open surgery. This can result in reduced pain, swelling, and scarring, as well as faster healing and recovery times for patients.
5. Minimal scarring: Laser incisions are often smaller and more precise, leading to minimal scarring. This is particularly important for cosmetic procedures or surgeries performed in visible areas.
6. Reduced hospital stay: Laser surgery is often performed on an outpatient basis, allowing patients to return home on the same day. This reduces the need for an extended hospital stay and associated costs.
7. Lower risk of complications: Laser surgery can potentially reduce the risk of certain complications, such as wound infection, blood loss, and damage to surrounding tissues.
However, it’s important to note that not all surgical procedures can be performed using lasers, and the suitability of laser surgery depends on the specific condition and the expertise of the surgeon. In some cases, traditional open surgery may still be the preferred option. It’s best to consult with a healthcare professional or surgeon to determine the most appropriate surgical approach for your specific situation.
ANAL FISSURES are tears, or cracks, in your anus. Fissures are sometimes confused with hemorrhoids. These are inflamed blood vessels in, or just outside, the anus. Both fissures and hemorrhoids often result from passing hard stool.
Causes
Fissures result from the stretching of your anal mucosa beyond its normal capacity. This often happens when stools are hard due to constipation. Once the tear happens, it leads to repeated injury. The exposed internal sphincter muscle beneath the tear goes into a spasm. This causes severe pain. The spasm also pulls the edges of the fissure apart, making it difficult for your wound to heal. The spasm then leads to further tearing of the mucosa when you have bowel movements. This cycle leads to the development of a chronic anal fissure in approximately 40% of patients.
Symptoms
You may have these symptoms with an anal fissure:
Pain during and after a bowel movement
Visible tear or cut in the area
Bright red bleeding during or after a bowel movement
Risk factors
Certain factors raise the risk for anal fissures, including:
Constipation with straining to pass hard stool
Eating a low-fiber diet
Intense diarrhea
Recent weight loss surgery, because it leads to frequent diarrhea
Vaginal childbirth
Minor trauma, especially trauma caused by high-level mountain biking
Any inflammatory condition of the anal area.
Anal fissures may also result from inflammatory bowel disease, surgery, or other medical treatments that affect bowel movements or the anus.
Diagnosis
Your healthcare provider will make a diagnosis based on:
Your personal health history
Your description of the symptoms
Rectal exam
Because other conditions can cause symptoms similar to an anal fissure, your healthcare provider might also order tests to find out whether there is blood in your stool.
Treatment
An acute anal fissure typically heals within 6 weeks with conservative treatment. Some disappear when constipation is treated. Anal fissures that last for 6 weeks or more are called chronic anal fissures. These fail conservative treatment and need a more aggressive, surgical approach.
Other treatments include:
Changing your diet to increase fiber and water, steps that will help regulate your bowel movements and reduce both diarrhea and constipation
Taking warm baths (SITZ BATH) for up to 20 minutes a day
Taking stool softeners, such as fiber supplements, as needed
Using topical medicines, such as nitrates or calcium blockers.
LASER treatment helps in healing by cauterizing fissure which promotes healing.
Having surgery, such as a lateral internal sphincterotomy. During the surgery, the pressure inside the anus is released. This allows more blood to flow through the area to heal and protect tissues.
Complications
Complications seen with anal fissures include:
Pain and discomfort
Reduced quality of life
Difficulty with bowel movements. Many people even avoid going to the bathroom because of the pain and discomfort it causes
Possible recurrence even after treatment
Clotting
Uncontrolled bowel movements and gas
Living with anal fissures
If you have an anal fissure, take these precautions to avoid making it worse and avoid recurrences:
Take all medicines as prescribed.
Get the recommended amount of fiber in your diet. Avoid constipation or large or hard bowel movements.
Drink enough water to stay well hydrated.
Maintain a routine bowel habit. Ask your healthcare provider about what this should be for you.
Avoid spicy foods while you have an anal fissure, because they may make symptoms worse.
Copyright 2022 © All Rights Reserved