Even successful treatments can be improved to provide patients with more options, including fewer side effects.
That’s the benefit of a major clinical trial (study) on rectal cancer treatment without radiation, announced in early June at the annual meeting of the American Society of Clinical Oncology (ASCO), the nation’s largest cancer society. The research also was announced on New England Medical Journal.
The study is led by gastrointestinal oncologist Deb Schrag, MD, MPH, medical director of Memorial Sloan Kettering Cancer Center (MSK).
Clinical trial results for rectal cancer treatment without radiation
The trial involved more than 1,100 people with locally advanced rectal cancer, meaning the cancer has not spread to other organs. Five years later, the study found that people who received a type of chemotherapy called FOLFOX alone before surgery performed as well as those who received both chemotherapy and radiation therapy before surgery. . Skipping radiation therapy can mean improved quality of life for patients, including preservation of fertility and sexual function.
Dr. Schrag said: “About 47,000 people are diagnosed with rectal cancer each year. Of these, approximately 20,000 patients with stage 2 or 3 cancer will benefit from this approach, which avoids chemotherapy, surgery, and radiation therapy. We believe we can receive it.”
Side effects of standard treatment for rectal cancer
People diagnosed with rectal cancer usually receive intravenous (intravenous) or oral (into the mouth) radiation to the pelvic area in conjunction with 5FU chemotherapy. This strategy is known as chemoradiotherapy and is sometimes referred to as 5FUCRT. The next step is surgery to remove the tumor and additional chemotherapy to prevent the cancer from coming back, usually in distant organs.
“We have been using chemoradiotherapy since 1990 because it has had remarkable effects in reducing local recurrence rates in the pelvis,” says Dr. Schrag. “This is very important because pelvic recurrence of rectal cancer is difficult to treat and causes a lot of suffering. Since 2004, we have been using chemoradiotherapy before surgery.”
But Dr. Schrag and his colleagues wondered if they could achieve the same results without exposing patients to the side effects often associated with radiation in such a complex area of the human anatomy.
The rectum is the last 6 inches of the digestive system. It is located inside the pelvis, a close-knit neighborhood of bones and dense organs. Radiation to this area can have side effects such as damaging reproductive organs, causing infertility, and leading to early menopause in women.
“My colleagues and I are seeing more and more devastated young women with rectal cancer. The reason was that she would not be able to carry the pregnancy to term,” the doctor said. . Schlag says. “That was one of the big reasons why we looked for ways to help patients and whether we could achieve good outcomes without uniform radiation delivery.”
Dr. Schrag believes these issues are especially urgent today because more people are being diagnosed with rectal cancer at younger ages, when fertility concerns are especially important. MSK is a leader in understanding why rectal cancer is on the rise among young people and has established the Center for Juvenile Colorectal and Gastrointestinal Cancer, the world’s first center dedicated to their specific needs. Did.
Dr. Schrag says people facing rectal cancer are often worried about other long-term effects of radiation, which can impair (damage or weaken) bowel and sexual function.
There are also concerns about radiation and the bone marrow that makes blood. “Most of the bone marrow is made in the pelvis. Radiation of these bones can compromise the resilience of the bone marrow,” she says. “This is important because if the cancer returns, chemotherapy will be more difficult to administer if the bone marrow reserve is compromised,” she added.
PROSPECT Clinical Trial for Rectal Cancer: Replacing 5FUCRT with FOLFOX
Dr. Schrag and his colleagues decided to fundamentally change the standard of care to address concerns about side effects.
The seeds of the clinical trial idea began to germinate during an MSK Colorectal Service meeting where experts from various fields discussed complex cases of rectal cancer. “MSK colorectal surgeon Martin Weiser, MD; gastrointestinal oncologist Leonard Saltz, MD; radiologist Mark Golub, MD, and I have begun a pilot study to test the effectiveness of this idea.” Dr. Schrag says. “Although this was a small study of just 30 of his patients, it enabled us to persuade colleagues across the country to test this approach in randomized trials.”
The chemotherapy usually given after surgery for rectal cancer is called FOLFOX and includes drugs such as 5-fluorouracil (5FU), oxaliplatin, and leucovorin. Preliminary studies have shown that administering FOLFOX before surgery may also yield positive results, and Dr. Schrag confirmed this in a pilot trial.
She hypothesized that administering FOLFOX alone before surgery, without radiation therapy, could provide patients with outcomes as good as standard treatment.
The trial, named PROSPECT, had two parts. In one group, FOLFOX chemotherapy was used before surgery and radiotherapy was used only if response to FOLFOX alone was insufficient (this occurred in less than 10% of patients). The other arm received chemoradiotherapy before surgery.
More than 1,100 patients were divided evenly between the two arms, with patients attending medical centers across the United States and Canada.
Five years later, the results were clear. Patients who received only her FOLFOX before surgery performed as well as those who received chemoradiotherapy. The primary endpoints, including disease-free survival, overall survival, and cancer recurrence rate, were nearly identical between the two methods.
The new method also showed other advantages. For example, without the use of radiation, the number of patients requiring temporary stomas was reduced. An ostomy is a surgically made hole in the abdomen (abdomen) that allows waste to be transported into a bag outside the body. Ostomination is usually temporary for patients with rectal cancer that has not metastasized, but after treatment with a new method, fewer patients required a stomatoma at all, with a clear improvement in quality of life. Improved.
Some people may still need radiation therapy for rectal cancer
Dr. Schrag is careful to point out that although this new method provides new options for patients and doctors, preoperative radiation may still be preferred in some cases. “About 10% of cases did not have an adequate response to the FOLFOX regimen and were treated with chemoradiotherapy,” she says.
Also, administering FOLFOX chemotherapy alone before surgery may require a longer period of treatment and increase early side effects, including neuropathy such as numbness and sharp pain in the hands.
Chemotherapy and surgery have side effects, but this study shows there is a non-radiation option for rectal cancer patients, Schrag said. “Especially for people who are concerned about radiation affecting their fertility, the new FOLFOX therapy provides an alternative,” she added.
Successful treatment of patients without radiotherapy
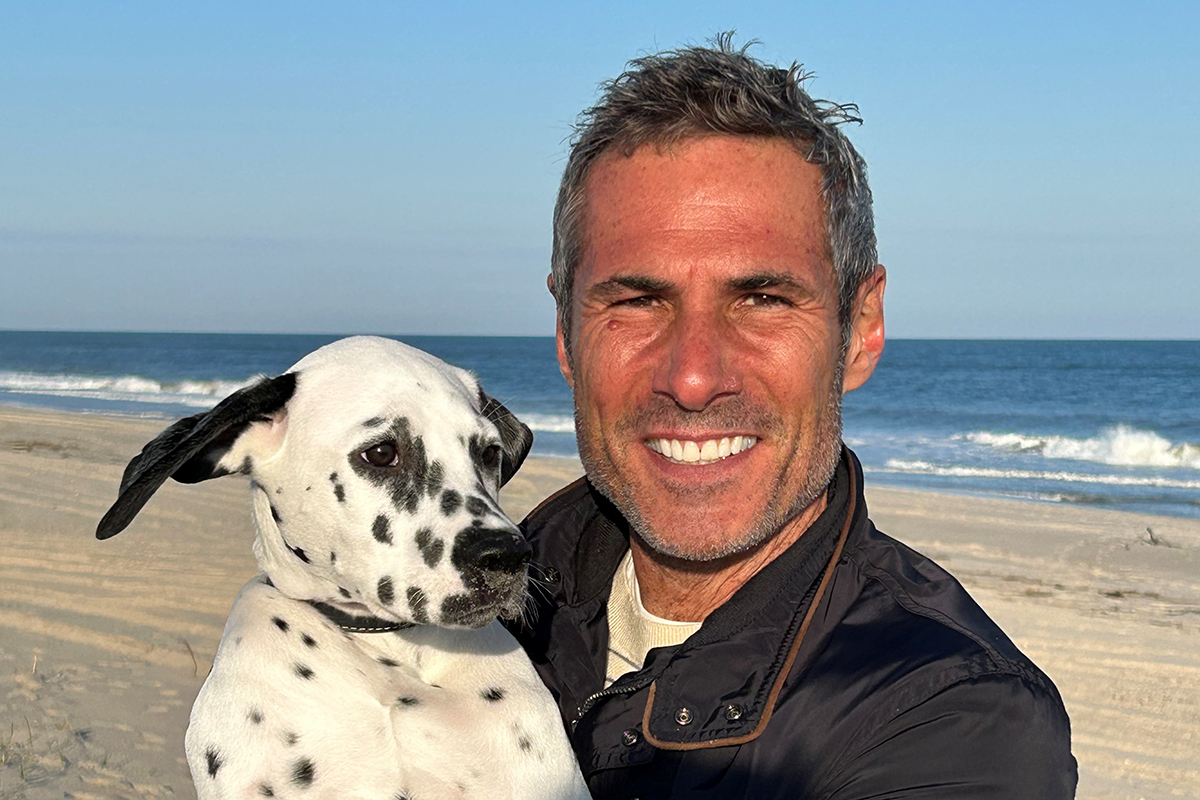
Mark Scardufa was relieved to be successfully treated for rectal cancer in the MSK clinical trial, skipping radiation therapy.
Having treatment options was important to Mark Scardufa. When he had his first colonoscopy at age 50, he felt healthy and had no symptoms. (At the time, the recommended age to start colorectal screening was 50 years old. The age for people at average risk was later lowered to 45 years old.)
Mark was shocked when tests revealed a stage 3 rectal cancer tumor. Mark spent much of his career leading government relations at a major pharmaceutical company and was well versed in medical issues. “I started at another hospital, but I stuck with MSK because it’s the gold standard.”
At MSK, Mark was treated by Drs. Saltz and Weiser. Mark immediately felt reassured by their compassion and concern for his quality of life, he said. “I was planning a big 50th birthday party in Italy, and Dr. Saltz said, ‘Go and have fun.’ We’ll start when you get back.'” With family and friends I was able to spend time there and it made a huge difference.”
When Mark returned, Drs. Saltz and Weiser told him about a clinical trial for a non-radiation treatment. “I had heard from some people about the side effects of radiation therapy,” Mark says. “I was so happy to have the opportunity to just have FOLFOX and surgery without having to undergo radiation therapy.”
In Mark’s case, the side effects from chemotherapy were mild. “Most people didn’t know I had cancer,” he says. “I was very passionate about not having to lose my hair to radiation and continued to travel frequently for work.” After recovering from the surgery, Mark regained his health and the clinical trial was definitely going to help his care. He says it was the right choice.
“I’m a huge fan of MSK and have told several other people facing cancer to go to MSK as well. I felt a real bond with the doctors.”
Rectal cancer treatment without radiation could help rural patients
This new method could also benefit patients who face geographic challenges in addition to cancer diagnosis.
“If you live in Idaho, Montana, or many other rural areas in the United States, you may be hours away from receiving radiation treatment,” Dr. Schrag says. Chemoradiotherapy requires 28 daily visits over five and a half weeks. In comparison, with FOLFOX he needs about 6 visits over 12 weeks. “For some people, schedule and convenience are important.”
The benefits are expanding globally, Schrag said, as some countries lack radiotherapy facilities. “In some parts of the world, access to radiation is very limited. Chemotherapy may be a more accessible alternative.”
Collaboration is the key to breakthrough discoveries
The study was funded by the National Cancer Institute, a federal initiative that is part of the National Institutes of Health. “This is taxpayer money that you are working for,” Dr. Schrag said. “This is the kind of work that is only funded by the government because there are no commercial sponsors.”
We were able to leverage these resources to accomplish the PROSPECT exam “thanks to strong leadership from a variety of disciplines,” she added. “Treatment of rectal cancer is a team sport.”
The PROSPECT team included Dr. Weiser (Colorectal Surgery); Ellen Hollywood, RNP (Nursing); Dr. Saltz (Medical Oncology). Dr. Karin Goodman (Radiation Oncology, currently at Mount Sinai). Dr. Golub (Radiology). Dr. Jinlu Xia (Pathology).
Dr. Schrag also looks forward to “the next generation of MSK researchers, including gastrointestinal oncologist Andrea Czerczek, MD.” gastrointestinal oncologist Rona Yeager, MD; Gastrointestinal oncologist Dr. Michael Foote. Surgical oncologist Josh Smith, MD, PhD, et al. She believes they will “usher in the next generation of clinical trials that will further improve outcomes for patients with rectal cancer.”
Dr. Schrag said he is deeply grateful to the courageous patients who participated in the trial. “It’s not easy to say to a patient, ‘Why don’t you just skip a treatment that’s been used for over 20 years?'” she says. “My hope is that this treatment will provide new options for rectal cancer patients and their doctors. MSK’s mission is to continue pushing the boundaries to make a meaningful difference for patients.”
Disclosure: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award numbers U10CA180821, U10CA180882, UG1CA189823 (to the Oncology Clinical Trials Alliance), UG1CA232760, UG1CA233180, UG1CA233290, UG1CA233329, UG1 Supported by CA233373, P30 CA008748, P30CA006516, U10CA180863, CCS#707213 (CCTG), U10CA180820 (ECOG-ACRIN), U10CA180868 (NRG), and U10CA180888 (SWOG), and Swiss Clinical Cancer Research Group (SAKK).
